You bought an otoscope. You looked in your kid’s ear. You saw red. Now you’re googling “red eardrum emergency room?” at 10 PM while your child plays happily in the next room.
Let me save you some anxiety: not all redness means infection. But some redness absolutely does. Here’s how to tell the difference.
The Anatomy Lesson Nobody Gave You
Your eardrum (tympanic membrane, if we’re being fancy) should look like a pearl. Slightly gray, slightly translucent, with a tiny cone of light reflecting when you angle the otoscope correctly. It’s delicate tissue stretched tight like a drum skin — hence the name.
When it’s healthy, you can sometimes see through it. The tiny bones of the middle ear (malleus, incus, stapes) might be faintly visible behind the membrane. This is normal. This is what you’re looking for when everything’s fine.
Why Eardrums Turn Red (Five Possibilities)
1. Your Kid Just Cried for Ten Minutes
Crying increases blood flow everywhere, including the ears. The eardrum gets extra blood supply, looks pinker than usual. You check because they were crying about ear pain, but the redness is actually from the crying itself.
How to tell: Wait 15 minutes. Check again. If the redness fades significantly, it was just increased blood flow from crying/screaming.
Action: Monitor. Give pain relief if needed. If pain continues for hours or worsens, then reassess.
2. Wax is Blocking Your View
Earwax is yellowish-brown. But when light shines through it from your otoscope, it can cast a reddish shadow on the eardrum behind it. You think you’re seeing a red eardrum, but you’re actually seeing normal tissue through a wax filter.
How to tell: Look for the actual wax buildup in the ear canal before you reach the eardrum. If there’s significant wax, you might not be seeing the drum clearly at all.
Action: Clean the wax (gently, with drops, never with Q-tips deep in the canal). Check again when you can see clearly.
3. The Angle Is Wrong
This was my problem for the first month. I’d angle the otoscope wrong, creating shadows that looked like dark spots or redness. The light needs to hit the eardrum straight on to see true color.
How to tell: Move the otoscope slightly — adjust the angle while looking. If the “redness” moves or changes dramatically with tiny movements, it’s probably a shadow or reflection issue.
Action: Practice on healthy ears when there’s no crisis. Learn what the right angle looks like so you recognize it during actual problems.
4. Outer Ear Inflammation (Not the Drum)
Sometimes the ear canal itself is red and inflamed — from swimmer’s ear, irritation, or early infection. You see redness as you look down the canal and assume it’s the eardrum, but the drum is actually fine.
How to tell: Follow the ear canal visually from the opening to the eardrum. Is the redness on the canal walls (the tunnel you’re looking through) or on the drum itself (the membrane at the end)?
Action: Outer ear infections (otitis externa) need different treatment than middle ear infections. Still see a doctor, but it’s useful to know the difference.
5. Actual Middle Ear Infection
This is the one you’re worried about. The eardrum is genuinely red, often uniformly so. It might also be bulging outward (pushed by fluid/pus behind it). You might see fluid level or bubbles behind the membrane. This is not subtle — it’s obvious when you know what you’re looking for.
How to tell:
- Uniform redness across the entire drum
- Drum appears pushed outward (bulging)
- Lost transparency (can’t see through it anymore)
- Visible fluid behind the membrane
- Pain that’s persistent and worsening
Action: Doctor visit needed. Probably antibiotics. Don’t wait days on this one.
The Real Red Flags (Pun Intended)
Stop reading, go to urgent care right now if you see:
A hole in the eardrum: Not redness — an actual perforation, opening, or tear. Looks like a dark spot that shouldn’t be there.
Blood or pus draining: If fluid is actively coming out, the drum has likely perforated or there’s a serious infection.
Complete blockage: If swelling is so severe you can’t even see past the ear canal, that’s an emergency-level infection.
Extremely bulging drum: Not just slightly full — dramatically pushed outward, about to burst. This needs immediate medical attention.
What I Actually Do When I See Redness
Here’s my decision tree, developed after three years of checking my daughter’s ears:
Step 1: Note the time and what my kid was doing. Just crying? Playing normally? Actual pain complaints?
Step 2: Check the other ear. If both are equally “red,” it’s probably not an infection (infections rarely perfectly mirror each other). More likely crying, lighting, or my technique.
Step 3: Look at my reference photo. I took pictures of Emma’s healthy ears when she was well. I compare to the baseline. Is this actually redder, or am I just paranoid because she said her ear hurt?
Step 4: Wait 30 minutes if symptoms are mild. Give pain relief (ibuprofen). Check again. If redness persists and pain continues, I’m more concerned. If redness faded, it was probably not an infection.
Step 5: Check for the “big three” infection signs:
- Is the redness uniform and obvious?
- Is the drum bulging?
- Is there visible fluid behind it?
If yes to two or more: we’re going to the doctor.
If no to all three: monitor at home, recheck in the morning.
The Photo Trick That Saved Me Money
I started taking photos through the otoscope lens of what I’m seeing. Not because I’m showing them to the doctor (though I have done that via patient portal, and it was useful). Because I can compare.
Is the redness I’m seeing tonight worse than what I photographed two hours ago? Stable? Better? Having that visual record eliminates the “am I remembering this accurately?” problem.
Most smartphone cameras can get decent shots through an otoscope lens if you hold steady and get the right angle. I keep a folder on my phone: “Emma’s Ears.” Sounds weird, but it’s been incredibly valuable for tracking whether problems are worsening or improving.
What Doctors Actually Want to Know
When I call the pediatrician’s nurse line, here’s what gets me taken seriously versus dismissed:
Bad: “Her ear looks red.”
Good: “I looked with an otoscope. Her left ear shows uniform redness across the eardrum with what looks like fluid behind it. The drum appears slightly bulging. She’s had worsening pain for four hours that ibuprofen isn’t touching. Right ear looks normal for comparison.”
That second version gets me same-day appointments. The first gets “give it 24 hours and call back.”
Being specific about what you’re actually seeing — not just “it looks infected” — changes how medical professionals respond to you. You’re giving them useful diagnostic information instead of vague worry.
The Confidence That Comes With Practice
I’m not a doctor. I’m never going to be as skilled at this as a pediatrician who’s examined 10,000 ears. But I’m pretty good at knowing when my daughter’s ear doesn’t look infected, which is most of the time.
That confidence — the ability to look and think “okay, this doesn’t look concerning, we can wait until morning” — has been worth every penny I paid for the otoscope.
Because the alternative is the 11 PM urgent care visit for every earache, the three-hour wait in a room full of actually sick people, the exhausted kid who can’t go to school tomorrow because we were up until 2 AM getting seen for something that turned out to be ear pain from jaw tension.
I’m not replacing doctors. I’m making better decisions about when to see doctors.
The One Thing I Wish I’d Known Earlier
Different kids have different baseline ear appearances. Emma’s eardrums have always been slightly pinker than the textbook “pearl gray.” For the first six months with the otoscope, I thought every slight pink tinge was an infection. I took her to the doctor three times before the pediatrician said, “Her baseline is just slightly pink. This is normal for her.”
Now I know what her normal looks like. Which means I can recognize her abnormality.
That’s why I keep saying: look at healthy ears regularly. Establish baseline. Know what normal is so you can identify abnormal with confidence.
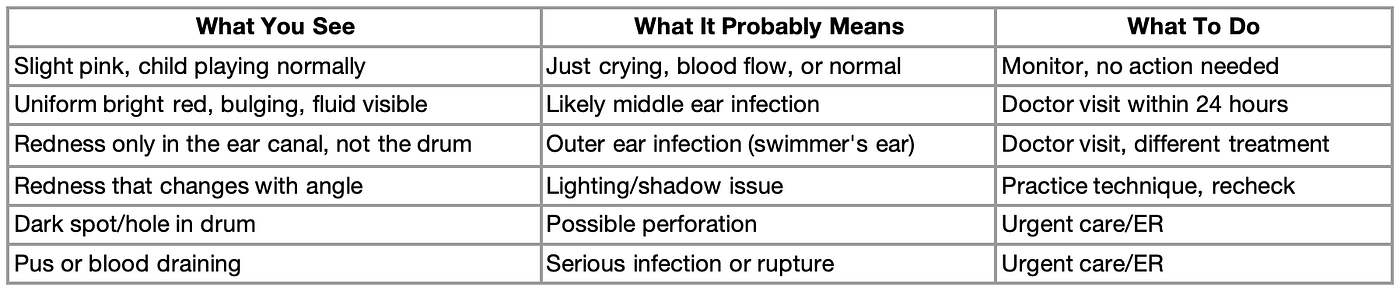
Quick Reference Guide
Save this for midnight panic googling:
Press enter or click to view image in full size
Bottom Line
Red doesn’t automatically equal infection. Context matters. Behavior matters. Other symptoms matter. The otoscope is a tool that provides information — you still need judgment to interpret that information.
But here’s what it absolutely does: it eliminates the complete uncertainty. Instead of “I have no idea if this is serious,” you have actual visual information to base decisions on.
That’s not nothing. That’s the difference between panicked ER visits at midnight and confident home monitoring until morning. For parents of kids with recurring ear issues, that peace of mind is priceless.
MediWares Portable Otoscope ($59.99): Fiber optic lighting, multiple specula sizes, rechargeable battery. Because 2 AM ear pain shouldn’t mean complete guesswork. Learn more at MediWares.com





Comments