1. Introduction
Dengue (breakbone fever) is a mosquito-borne infection caused by Dengue virus (DENV), a Flavivirus (Others see West Nile Virus (WNV), Japanese Encephalitis Virus (JEV), Yellow Fever Virus (YFV) and Zika Virus (ZIKV).) that is characterized by fever, severe headache, muscle and joint pain, nausea and vomiting, eye pain, and rash. Severe forms of the disease, dengue hemorrhagic fever and dengue shock syndrome, principally affect children.
Dengue virus is transmitted by female mosquitoes mainly of the species Aedes aegypti and, to a lesser extent, Ae. albopictus. This mosquito also transmits chikungunya, yellow fever and Zika infection. Dengue is widespread throughout the tropics, with local variations in risk influenced by rainfall, temperature and unplanned rapid urbanization.
The first record of a case of probable dengue fever is in a Chinese medical encyclopedia from the Jin Dynasty (265–420 AD) which referred to a “water poison” associated with flying insects. The first recognized Dengue epidemics occurred almost simultaneously in Asia, Africa, and North America in the 1780s, shortly after the identification and naming of the disease in 1779. The first confirmed case report dates from 1789 and is by Benjamin Rush, who coined the term "breakbone fever" because of the symptoms of myalgia and arthralgia. The viral etiology and the transmission by mosquitoes were only deciphered in the 20th century. The socioeconomic impact of World War II resulted in increased spread globally. Nowadays, about 2.5 billion people, or 40% of the world's population, live in areas where there is a risk of dengue transmission. Dengue spread to more than 100 countries in Asia, the Pacific, the Americas, Africa, and the Caribbean.
2. Signs and Symptoms
After being bitten by a mosquito carrying the dengue virus, the incubation period ranges from 3 to 14 (usually 4 to 7) days before the signs and symptoms of dengue appear. Dengue occurs in two forms:
Dengue Fever:
Dengue fever is a severe, flu-like illness that affects infants, young children and adults, but seldom causes death. Dengue should be suspected when a high fever (40°C/104°F) is accompanied by 2 of the following symptoms: severe headache, pain behind the eyes, muscle and joint pains, nausea, vomiting, swollen glands or rash. Symptoms usually last for 2–7 days, after an incubation period of 4–10 days after the bite from an infected mosquito.
Recognition of Dengue fever:
- Sudden onset of high fever
- Severe headache (mostly in the forehead)
- Pain behind the eyes which worsens with eye movement
- Body aches and joint pains
- Nausea or vomiting
Dengue Haemorrhagic Fever:
Dengue hemorrhagic fever (DHF) is a potentially deadly complication due to plasma leaking, fluid accumulation, respiratory distress, severe bleeding, or organ impairment. Warning signs occur 3–7 days after the first symptoms in conjunction with a decrease in temperature (below 38°C/100°F) and include: severe abdominal pain, persistent vomiting, and rapid breathing, bleeding gums, fatigue, restlessness and blood in vomit. The next 24–48 hours of the critical stage can be lethal; proper medical care is needed to avoid complications and risk of death.
Recognition of Dengue Haemorrhagic Fever (DHF):
Symptoms similar to dengue fever plus, any one of the following:
- Severe and continuous pain in abdomen
- Bleeding from the nose, mouth and gums or skin bruising
- Frequent vomiting with or without blood
- Black stools, like coal tar
- Excessive thirst (dry mouth)
- Pale, cold skin
- Restlessness, or sleepiness
3. About Dengue Virus
Dengue virus (DENV), a member of the family Flaviviridae, is a major human pathogen transmitted by mosquitoes. There are four antigenically different serotypes of the virus (although there is report of 2013 that a fifth serotype has been found): These four subtypes are different strains of dengue virus that have 60-80% homology between each other. The major difference for humans lies in subtle differences in the surface proteins of the different dengue subtypes. Infection induces long-life protection against the infecting serotype, but it gives only a short time cross protective immunity against the other types. The first infection cause mostly minor disease, but secondary infections has been reported to cause severe diseases (DHF or DSS) in both children and adults. This phenomenon is called Antibody-Dependent Enhancement.
Each of the four serotypes of DENV (DENV-1, DENV-2, DENV-3 and DENV-4) is capable of causing the full spectrum of clinical manifestations following DENV infection, ranging from an asymptomatic infection to dengue fever (DF) and the most severe disease, dengue haemorrhagic fever (DHF) and dengue shock syndrome (DSS).
DENV is a 50-nm virus enveloped with a lipid membrane (Figure 1a). There are 180 identical copies of the envelope (E) protein attached to the surface of the viral membrane by a short transmembrane segment. The virus has a genome of about 11000 bases that encodes a single large polyprotein that is subsequently cleaved into several structural and non-structural mature peptides. The 11-kb positive sense RNA genome encodes 3 structural proteins (capsid, prM, and E) and 7 nonstructural proteins (NS1, NS2a, NS2b, NS3, NS4a, NS4b, and NS5) (Figure 1a). The virus particle consists of an RNA-capsid protein complex, surrounded by a bilayer lipid membrane. The proteins present on the surface of the dengue immature virus are the E and prM. The mature virus surface, on the other hand, contains E and M proteins (a cleaved derivative of prM).
See All Products of Dengue Viral Antigen

Figure 1. Structure of Dengue Virus particle. The surface protein (a) and Envelope glycoproteins are showed (b,c).
4. Life Cycle of Dengue Virus
The dengue viral replication process begins when the virus attaches to a human skin cell (Figure 2). After this attachment, the skin cell's membrane folds around the virus and forms a pouch that seals around the virus particle. This pouch is called an endosome. A cell normally uses endosomes to take in large molecules and particles from outside the cell for nourishment. By hijacking this normal cell process, the dengue virus is able to enter a host cell. Once the virus has entered a host cell, the virus penetrates deeper into the cell while still inside the endosome. Researchers have learned that two conditions are needed for the dengue virus to exit the endosome: The endosome must be deep inside the cell where the environment is acidic. The endosomal membrane must gain a negative charge. These two conditions allow the virus envelope to fuse with the endosomal membrane, and that process releases the dengue nucleocapsid into the cytoplasm of the cell. In the cytoplasm, the nucleocapsid opens to uncoat the viral genome. This process releases the viral RNA into the cytoplasm. The viral RNA then hijacks the host cell's machinery to replicate itself. The virus uses ribosomes on the host's rough endoplasmic reticulum (ER) to translate the viral RNA and produce the viral polypeptide. This polypeptide is then cut to form the ten dengue proteins. The newly synthesized viral RNA is enclosed in the C proteins, forming a nucleocapid. The nucleocapsid enters the rough ER and is enveloped in the ER membrane and surrounded by the M and E proteins. This step adds the viral envelope and protective outer layer. The immature viruses travel through the Golgi apparatus complex, where the viruses mature and convert into their infectious form. The mature dengue viruses are then released from the cell and can go on to infect other cells.
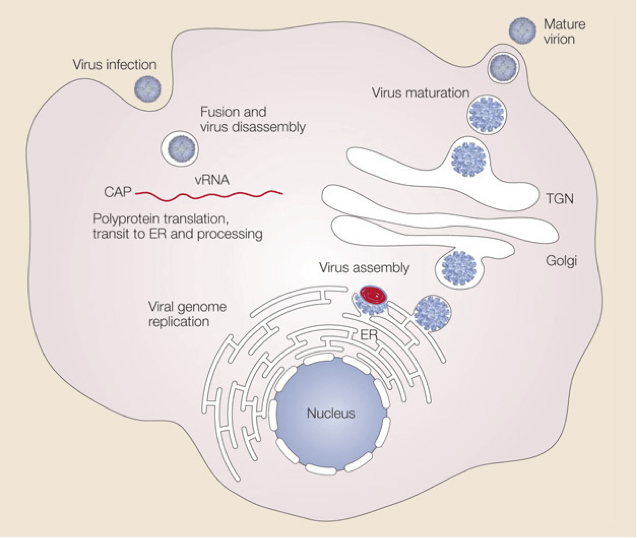
Figure 2. Life cycle of Dengue virus
5. Diagnosis, Treatment and Prevention
Diagnosis:
Dengue can be diagnosed by isolation of the virus, by serological tests, or by molecular methods. Diagnosis of acute (on-going) or recent dengue infection can be established by testing serum samples during the first 5 days of symptoms and/or early convalescent phase (more than 5 days of symptoms). Acute infection with dengue virus is confirmed when the virus is isolated from serum or autopsy tissue specimens, or the specific dengue virus genome is identified by RT–PCR from serum or plasma, cerebrospinal fluid, or autopsy tissue specimens during an acute febrile illness. Acute infections can also be laboratory confirmed by identification of dengue viral antigen or RNA in autopsy tissue specimens by immunofluorescence or immunohistochemical analysis, or by seroconversion from negative to positive IgM antibody to dengue or demonstration of a fourfold or greater increase in IgG antibody titers in paired (acute and convalescent) serum specimens.
See Dengue ELISA Kit and Dengue RDT Products
Treatment:
There is no specific treatment for dengue fever.
For severe dengue, medical care by physicians and nurses experienced with the effects and progression of the disease can save lives – decreasing mortality rates from more than 20% to less than 1%. Maintenance of the patient's body fluid volume is critical to severe dengue care.
Prevention:
In late 2015 and early 2016, the first dengue vaccine, Dengvaxia (CYD-TDV) by Sanofi Pasteur, was registered in several countries for use in individuals 9-45 years of age living in endemic areas. At present, the main method to control or prevent the transmission of dengue virus is to combat vector mosquitoes.
References
- Zhang Q, Hunke C, Yau Y H, et al. The stem region of premembrane protein plays an important role in the virus surface protein rearrangement during dengue maturation[J]. Journal of Biological Chemistry, 2012, 287(48): 40525-40534.
- Rodenhuis-Zybert I A, Wilschut J, Smit J M. Dengue virus life cycle: viral and host factors modulating infectivity[J]. Cellular and molecular life sciences, 2010, 67(16): 2773-2786.
- Modis Y, Ogata S, Clements D, et al. Structure of the dengue virus envelope protein after membrane fusion[J]. Nature, 2004, 427(6972): 313-319.
- Whitehead S S, Blaney J E, Durbin A P, et al. Prospects for a dengue virus vaccine[J]. Nature Reviews Microbiology, 2007, 5(7): 518-528.
- Zhang X, Ge P, Yu X, et al. Cryo-EM structure of the mature dengue virus at 3.5-Å resolution[J]. Nature structural & molecular biology, 2013, 20(1): 105-110.




Comments