Diagnosing an enlarged prostate, medically termed benign prostatic hyperplasia (BPH), involves a systematic approach that includes medical history assessment, physical examination, and often specific tests to confirm the condition and rule out other potential causes of urinary symptoms.
Here’s a detailed overview of the diagnostic process:
1. Medical History and Symptoms Assessment:
— The first step typically involves discussing symptoms with a healthcare provider. Symptoms of an enlarged prostate can include frequent or urgent need to urinate, difficulty starting or maintaining urination, weak urine stream, dribbling after urination, and feeling of incomplete emptying of the bladder.
— Information about the onset, duration, and severity of symptoms is important. Additionally, any history of urinary tract infections, kidney problems, or previous prostate issues is noted.
2. Physical Examination:
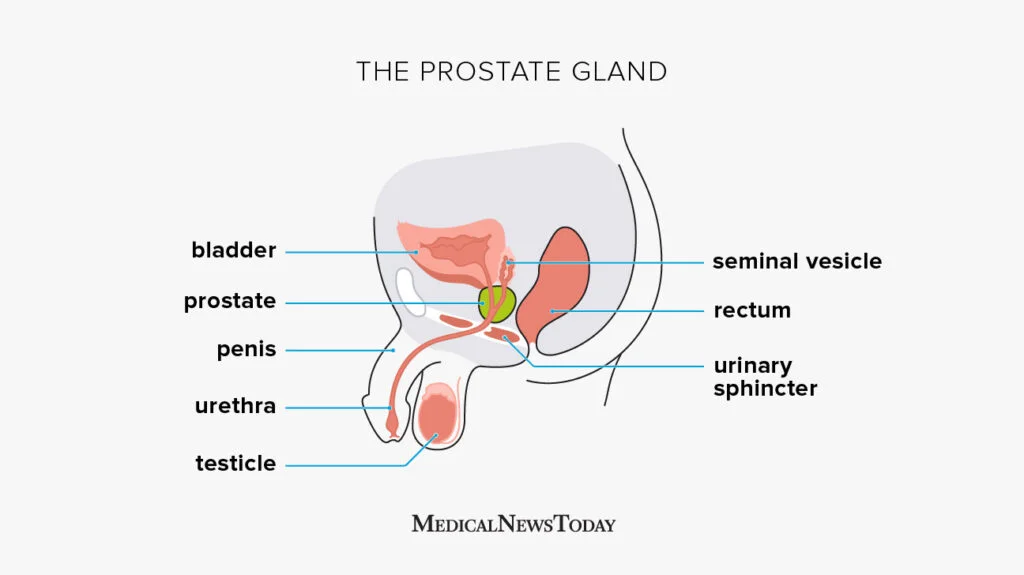
— A physical examination often includes a digital rectal examination (DRE), where the doctor inserts a gloved, lubricated finger into the rectum to feel the prostate gland. This allows the doctor to assess the size, shape, and consistency of the prostate gland.
3. Prostate-Specific Antigen (PSA) Test:
— A blood test to measure PSA levels may be done. PSA is a protein produced by the prostate gland, and elevated levels can sometimes indicate prostate inflammation, infection, enlargement (BPH), or even prostate cancer. However, PSA levels alone are not diagnostic of BPH.
4. Urinalysis and Urine Culture:
— Urinalysis may be performed to check for signs of infection or other abnormalities in the urine. A urine culture may also be done if there are symptoms suggesting a urinary tract infection.
5. International Prostate Symptom Score (IPSS):
— This is a questionnaire used to assess the severity of urinary symptoms and their impact on daily life. It helps to quantify and track symptoms over time.
6. Post-Void Residual (PVR) Measurement:
— This test measures the amount of urine left in the bladder after urination. It can be done using ultrasound, where a device is placed on the abdomen to visualize the bladder, or via a catheter inserted into the bladder.
7. Transrectal Ultrasound (TRUS):
— In some cases, a TRUS may be performed to get detailed images of the prostate gland. This imaging technique uses sound waves to create pictures of the prostate and surrounding tissues.
8. Cystoscopy:
— If there are concerns about other possible causes of urinary symptoms or if treatment options need to be explored further, a cystoscopy may be performed. This involves inserting a thin, flexible tube with a camera (cystoscope) into the urethra to examine the bladder and prostate.
Through a combination of these diagnostic methods, healthcare providers can accurately diagnose an enlarged prostate, assess its severity, and determine the most appropriate treatment plan tailored to the individual patient’s needs. Early diagnosis and management of BPH are crucial to alleviate symptoms, prevent complications like urinary retention or bladder stones, and maintain good urinary tract health.





Comments