Differentiating between a urinary tract infection (UTI) and interstitial cystitis (IC) can be challenging, as both conditions share several similar symptoms. However, they have distinct characteristics and underlying causes that can help in making an accurate diagnosis. Here’s a breakdown to help differentiate between the two:
1. Understanding the Conditions
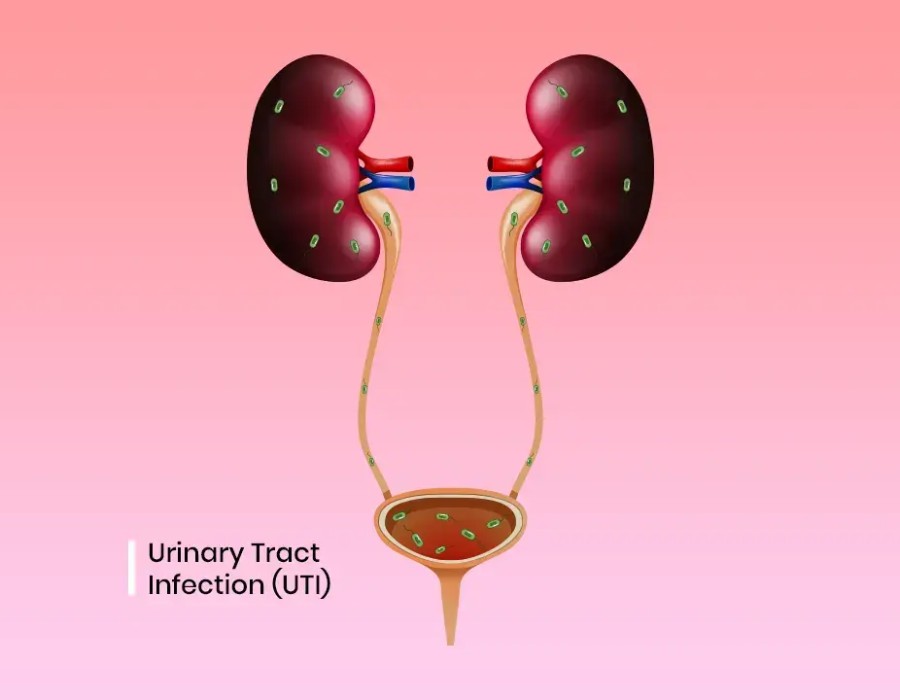
Urinary Tract Infection (UTI):
A UTI is an infection caused by bacteria entering the urinary tract. It can affect any part of the urinary system, including the kidneys, bladder, ureters, and urethra. UTIs are often acute and respond well to antibiotics.
Interstitial Cystitis (IC):
IC, also known as painful bladder syndrome, is a chronic condition characterized by bladder pain and discomfort without an obvious bacterial infection. The exact cause of IC is not well understood, and it is often a diagnosis of exclusion after other conditions have been ruled out.
2. Symptoms Comparison
Symptoms of a UTI:
- Frequent Urination: A need to urinate more often than usual.
- Urgency: A strong, persistent urge to urinate.
- Pain or Burning Sensation: Pain or a burning feeling during urination.
- Cloudy or Strong-Smelling Urine: Urine may appear cloudy, dark, or have a strong odor.
- Hematuria: Presence of blood in the urine, which may make it appear pink or red.
- Pelvic Pain: Discomfort or pain in the lower abdomen or pelvic area.
- Fever and Chills: In more severe cases, systemic symptoms like fever and chills can occur, especially if the infection has spread to the kidneys (pyelonephritis).
Symptoms of Interstitial Cystitis (IC):
- Chronic Pelvic Pain: Persistent pain or discomfort in the bladder or pelvic area that is not necessarily linked to urination.
- Frequent Urination: Frequent need to urinate, often in small amounts.
- Urgency: A sudden and strong need to urinate.
- Pain During or After Urination: Pain or discomfort during or after urination, but not necessarily a burning sensation.
- Bladder Pressure or Pain: Pressure or pain in the bladder that can worsen as the bladder fills.
- No Evidence of Infection: No bacterial growth in urine cultures, which is a key differentiator from a UTI.
3. Diagnostic Approach
For a UTI:
- Urine Analysis: A urinalysis can identify bacteria, white blood cells, and other indicators of infection.
- Urine Culture: Culturing the urine can determine the specific bacteria causing the infection and the appropriate antibiotic treatment.
For Interstitial Cystitis (IC):
- Exclusion of Other Conditions: Diagnosis often involves ruling out other potential causes of bladder symptoms, including UTIs and other bladder disorders.
- Cystoscopy: A procedure where a thin tube with a camera is inserted into the bladder to examine its lining. It can help rule out other conditions and sometimes reveal characteristic features of IC.
- Bladder Biopsy: In some cases, a biopsy may be performed during cystoscopy to assess for characteristic changes in the bladder tissue.
4. Treatment Differences
UTI Treatment:
- Antibiotics: Typically treated with a course of antibiotics. Improvement is usually seen within a few days.
Interstitial Cystitis Treatment:
- Lifestyle Changes: Dietary modifications, stress management, and avoiding irritants like caffeine and alcohol.
- Medications: May include pain relievers, antihistamines, and medications specifically for IC.
- Bladder Instillations: Solutions containing medication can be directly instilled into the bladder.
- Physical Therapy: For pelvic floor issues associated with IC.
- Other Therapies: Such as nerve stimulation or surgery in severe cases.
5. When to Seek Medical Advice
If you experience symptoms suggestive of a UTI or IC, it’s important to consult a healthcare provider for an accurate diagnosis and appropriate treatment. While UTIs can often be treated quickly with antibiotics, IC requires a more comprehensive approach to manage symptoms and improve quality of life.




Comments