Atrial fibrillation
Overview
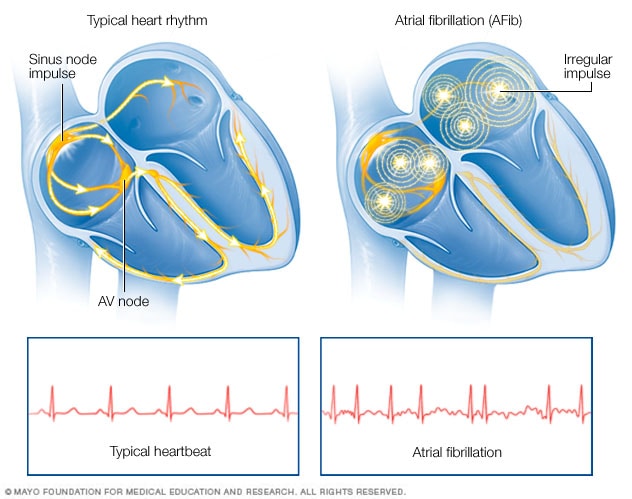
Atrial fibrillation is an irregular and often rapid heart rate that can increase your risk of strokes, heart failure and other heart-related complications.
During atrial fibrillation, the heart's two upper chambers (the atria) beat chaotically and irregularly — out of coordination with the two lower chambers (the ventricles) of the heart. Atrial fibrillation symptoms often include heart palpitations, shortness of breath and weakness.
Episodes of atrial fibrillation may come and go, or you may develop atrial fibrillation that doesn't go away and may require treatment. Although atrial fibrillation itself usually isn't life-threatening, it is a serious medical condition that sometimes requires emergency treatment.
A major concern with atrial fibrillation is the potential to develop blood clots within the upper chambers of the heart. These blood clots forming in the heart may circulate to other organs and lead to blocked blood flow (ischemia).
Treatments for atrial fibrillation may include medications and other interventions to try to alter the heart's electrical system.
Products & Services
Show more products from Mayo Clinic
Symptoms
Some people with atrial fibrillation have no symptoms and are unaware of their condition until it's discovered during a physical examination. Those who do have atrial fibrillation symptoms may experience signs and symptoms such as:
- Palpitations, which are sensations of a racing, uncomfortable, irregular heartbeat or a flip-flopping in your chest
- Weakness
- Reduced ability to exercise
- Fatigue
- Lightheadedness
- Dizziness
- Shortness of breath
- Chest pain
Atrial fibrillation may be:
- Occasional. In this case it's called paroxysmal (par-ok-SIZ-mul) atrial fibrillation. You may have symptoms that come and go, usually lasting for a few minutes to hours. Sometimes symptoms occur for as long as a week and episodes can happen repeatedly. Your symptoms might go away on their own or you may need treatment.
- Persistent. With this type of atrial fibrillation, your heart rhythm doesn't go back to normal on its own. If you have persistent atrial fibrillation, you'll need treatment such as an electrical shock or medications in order to restore your heart rhythm.
- Long-standing persistent. This type of atrial fibrillation is continuous and lasts longer than 12 months.
- Permanent. In this type of atrial fibrillation, the abnormal heart rhythm can't be restored. You'll have atrial fibrillation permanently, and you'll often require medications to control your heart rate and to prevent blood clots.
When to see a doctor
If you have any symptoms of atrial fibrillation, make an appointment with your doctor. Your doctor may order an electrocardiogram to determine if your symptoms are related to atrial fibrillation or another heart rhythm disorder (arrhythmia).
If you have chest pain, seek emergency medical assistance immediately. Chest pain could signal that you're having a heart attack.
Request an Appointment at Mayo Clinic
Causes
Atrial fibrillation
Atrial fibrillation is an irregular and often rapid heart rate that occurs when the two upper chambers of your heart experience chaotic electrical signals. The result is a fast and irregular heart rhythm. The heart rate in atrial fibrillation may range from 100 to 175 beats a minute. The normal range for a heart rate is 60 to 100 beats a minute.
Your heart is made up of four chambers — two upper chambers (atria) and two lower chambers (ventricles). Within the upper right chamber of your heart (right atrium) is a group of cells called the sinus node. This is your heart's natural pacemaker. The sinus node produces the signal that normally starts each heartbeat.
Normally, the signal travels through the two upper heart chambers, and then through a connecting pathway between the upper and lower chambers called the atrioventricular (AV) node. The movement of the signal causes your heart to squeeze (contract), sending blood to your heart and body.
In atrial fibrillation, the signals in the upper chambers of your heart are chaotic. As a result, they quiver. The AV node — the electrical connection between the atria and the ventricles — is bombarded with impulses trying to get through to the ventricles.
The ventricles also beat rapidly, but not as rapidly as the atria, as not all the impulses get through.
Possible causes of atrial fibrillation
Abnormalities or damage to the heart's structure are the most common cause of atrial fibrillation. Possible causes of atrial fibrillation include:
- High blood pressure
- Heart attack
- Coronary artery disease
- Abnormal heart valves
- Heart defects you're born with (congenital)
- An overactive thyroid gland or other metabolic imbalance
- Exposure to stimulants, such as medications, caffeine, tobacco or alcohol
- Sick sinus syndrome — improper functioning of the heart's natural pacemaker
- Lung diseases
- Previous heart surgery
- Viral infections
- Stress due to surgery, pneumonia or other illnesses
- Sleep apnea
However, some people who have atrial fibrillation don't have any heart defects or damage, a condition called lone atrial fibrillation. In lone atrial fibrillation, the cause is often unclear, and serious complications are rare.
Atrial flutter
Atrial flutter is similar to atrial fibrillation, but the rhythm in your atria is more organized and less chaotic than the abnormal patterns common with atrial fibrillation. Sometimes you may have atrial flutter that develops into atrial fibrillation and vice versa.
The risk factors for and the symptoms and causes of atrial flutter are similar to those of atrial fibrillation. For example, strokes are also a concern in someone with atrial flutter. As with atrial fibrillation, atrial flutter is usually not life-threatening when it's properly treated.
Risk factors
Certain factors may increase your risk of developing atrial fibrillation.
These include:
- Age. The older you are, the greater your risk of developing atrial fibrillation.
- Heart disease. Anyone with heart disease — such as heart valve problems, congenital heart disease, congestive heart failure, coronary artery disease, or a history of heart attack or heart surgery — has an increased risk of atrial fibrillation.
- High blood pressure. Having high blood pressure, especially if it's not well-controlled with lifestyle changes or medications, can increase your risk of atrial fibrillation.
- Other chronic conditions. People with certain chronic conditions such as thyroid problems, sleep apnea, metabolic syndrome, diabetes, chronic kidney disease or lung disease have an increased risk of atrial fibrillation.
- Drinking alcohol. For some people, drinking alcohol can trigger an episode of atrial fibrillation. Binge drinking may put you at an even higher risk.
- Obesity. People who are obese are at higher risk of developing atrial fibrillation.
- Family history. An increased risk of atrial fibrillation is present in some families.
Complications
Sometimes atrial fibrillation can lead to the following complications:
- Stroke. In atrial fibrillation, the chaotic rhythm may cause blood to pool in your heart's upper chambers (atria) and form clots. If a blood clot forms, it could dislodge from your heart and travel to your brain. There it might block blood flow, causing a stroke.
- The risk of a stroke in atrial fibrillation depends on your age (you have a higher risk as you age) and on whether you have high blood pressure, diabetes, a history of heart failure or a previous stroke, and other factors. Certain medications, such as blood thinners, can greatly lower your risk of a stroke or the damage to other organs caused by blood clots.
- Heart failure. Atrial fibrillation, especially if not controlled, may weaken the heart and lead to heart failure — a condition in which your heart can't circulate enough blood to meet your body's needs.
Prevention
To prevent atrial fibrillation, it's important to live a heart-healthy lifestyle to reduce your risk of heart disease. A healthy lifestyle may include:
- Eating a heart-healthy diet
- Increasing your physical activity
- Avoiding smoking
- Maintaining a healthy weight
- Limiting or avoiding caffeine and alcohol
- Reducing stress, as intense stress and anger can cause heart rhythm problems
- Using over-the-counter medications with caution, as some cold and cough medications contain stimulants that may trigger a rapid heartbeat





Comments