Prostate health becomes more critical with age, especially when someone notices changes or receives test results that need a closer look. Doctors may then suggest further checks to understand what is causing these changes. During this process, some men are diagnosed with prostate cancer, which requires careful guidance and clear discussions about treatment options.
After a diagnosis, people often want clear guidance on what to do next. For men with early-stage prostate cancer that is still limited to the prostate, robotic prostatectomy is one option a doctor may suggest. Learning how this procedure works can help you feel more prepared for what happens before, during, and after the surgery.
What Is Robotic Prostatectomy?
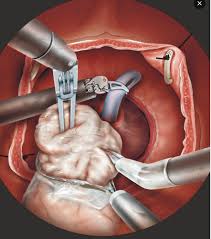
Robotic prostatectomy is a minimally invasive surgery used to remove the prostate gland in men with early-stage cancer that has not spread. During surgery, a robotic system helps the surgeon perform steady, precise movements, thereby protecting nearby tissues.
The surgery is done through a few minor cuts in the abdomen instead of one large opening. This approach may lead to less blood loss, fewer minor scars, and shorter hospital stays. The outcome depends on the stage of the cancer, the patient's overall health, and the surgeon's experience.
Who Can Undergo This Procedure?
Not everyone diagnosed with prostate cancer is advised to have surgery. Robotic prostatectomy is usually suggested for men with early-stage cancer that remains within the prostate. Doctors assess several factors, including age, existing health conditions, prostate size, and overall fitness, before recommending this approach.
Some people may benefit more from other options such as radiation therapy, hormone therapy, or careful monitoring. A detailed discussion with the doctor helps identify the most suitable plan for each person.
Step-by-Step Procedure
Understanding the steps involved in robotic prostatectomy can help patients feel more prepared. The procedure usually includes:
- Giving general anaesthesia to keep the patient asleep throughout the procedure
- Making a few minor cuts in the lower abdomen
- Placing a thin camera and robotic surgical tools through these cuts
- The surgeon is using a console to guide the robotic arms with steady, controlled movements
- Removing the prostate gland with care to protect nearby tissues
- Joining the bladder and urethra with delicate stitches
- Removing the instruments and closing the cuts
- Placing a urinary catheter to support healing during the early days
The surgeon performs each step to protect the surrounding nerves and structures.
Benefits of the Procedure
This approach offers several advantages over traditional open surgery. Learning about these benefits can help patients and their families feel more prepared. Some possible advantages include:
- More minor cuts and minimal scarring
- Less blood loss during the operation
- Lower chance of infection
- A shorter hospital stay and a quicker recovery
- Clearer visibility of tissues during the surgery
- Better chances of preserving urinary control and sexual function when possible
Outcomes vary for each person based on their health, cancer stage, and the surgeon's experience.
Risks and Possible Side Effects
Every surgery carries some risks, and this procedure is no different. Knowing the possible side effects can help patients feel better prepared. Some of these may include:
- Infection around the cuts
- Bleeding or blood clots
- Irritation or injury to nearby tissues
- Temporary urinary leakage during early recovery
- Changes in sexual function due to nerve irritation
Many of these effects improve over time with proper support. Guidance from the medical team and reassurance from family can also help during recovery.
Recovery and Aftercare
Recovery after this surgery takes time and involves both physical healing and day-to-day adjustments. Most patients return home within a couple of days, though full recovery may take longer. To support healing, doctors often advise patients to:
- Avoid heavy lifting or strenuous activities for a few weeks
- Take short walks to improve circulation
- Keep the surgical area clean and dry
- Attend follow-up visits to check healing and remove the catheter
- A doctor must be informed if fever, sharp pain, or difficulty in urinating is noticed.
These steps can help the body heal steadily. With the proper care and support, most men regain strength and gradually return to their routine.
Life After Surgery
Life after the surgery gradually becomes easier as the body heals. Many patients have questions about bladder control, sexual health, or returning to work. These are typical concerns and can be discussed with the doctor during follow-up visits. Most men return to their usual activities within four to six weeks, depending on their recovery.
Regular PSA tests help track postoperative progress. In some cases, doctors may suggest additional treatment such as radiation or hormone therapy. A balanced diet, light exercise, and steady support from family can make the recovery journey smoother.
Conclusion
This procedure is one of the treatment options available for men with early-stage prostate cancer. Knowing the steps involved, along with their benefits, risks, and recovery process, can help patients feel more at ease. Clear guidance also supports families as they make informed decisions together. At Nanavati Max Super Speciality Hospital, specialists offer careful evaluations and steady support to help patients choose the approach that suits their needs.




Comments