Genetically engineered drugs are introduced into host cells such as Escherichia coli, yeast or mammalian cells through recombinant technology to construct engineering strains or cell strains, and then undergo specific expression, assembly, folding and post-translational modification processes to produce drugs with corresponding Bioactive macromolecules. Endogenous proteins derived from host cells are called host cell proteins (HCPs). Their composition is complex. Depending on the selected host cells and production processes, the isoelectric point (3-11), hydrophobicity, relative the molecular mass (generally 5000~250000) distribution varies significantly.
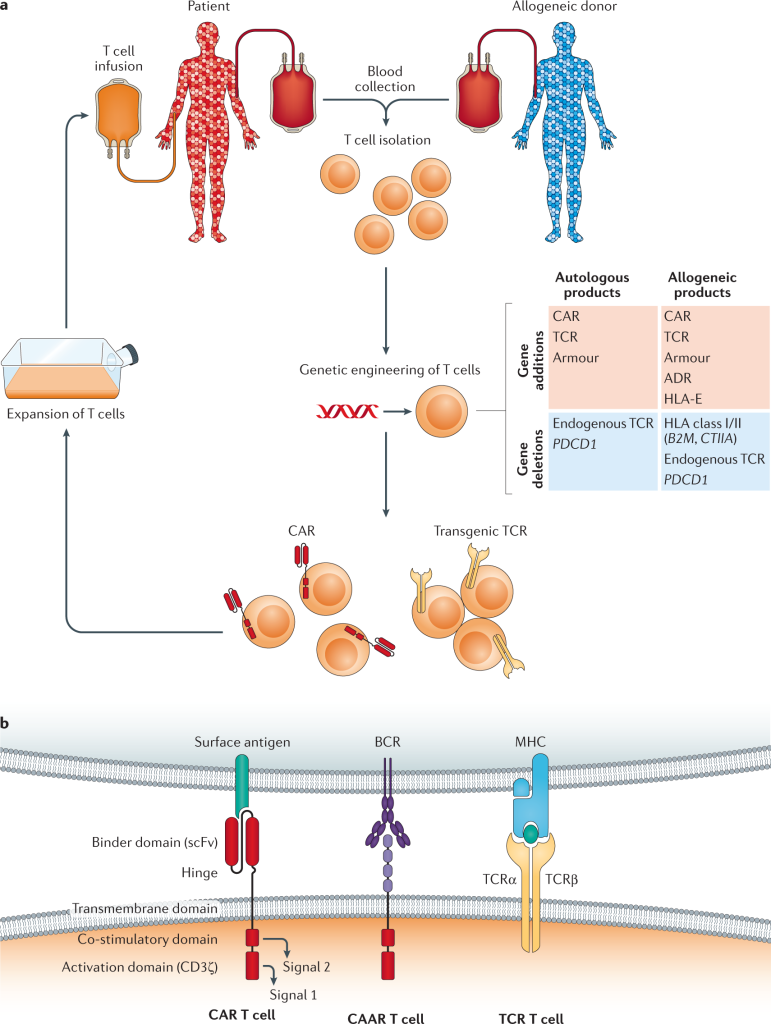
Figure 1. Autologous and allogeneic T cell immunotherapy.
Cellular HCPs in genetically engineered drugs may cause different human reactions when administered, because specific HCPs have potential “adjuvant effects”, generate immune responses against impurities in HCPs, or cause allergic reactions or even anaphylactic shock. In addition to safety issues, the presence of HCPs can also affect product quality. For example, HCPs can trigger aggregation or fragmentation of therapeutic proteins. In addition, it was found that certain HCPs promote the degradation of polysorbates, a type of non-ionic surfactant widely used in the preparation of buffers to stabilize proteins. The degradation of polysorbates will affect the stability of protein drugs. The protease activity in HCPs can also affect the protein composition in the culture supernatant, thereby affecting the subsequent protein purification process or the stability of long-term storage of protein drugs. In addition, HCPs may undergo post-translational modifications, making quantification and characterization more difficult. In view of the fact that cellular HCPs in genetically engineered drugs may cause safety and effectiveness issues, the detection of their removal efficiency and cell limit is an important parameter for drug release and clinical research, and is one of the critical product quality attributes (CQA) of drug quality control. Therefore, although only a few clinical adverse events have so far been attributed to HCPs impurities, in order to ensure product safety, HCPs must be accurately characterized and quantitatively analyzed through highly sensitive analytical methods.
Factors Influencing HCPs
The quantity and composition of HCPs are affected by the entire production process. Among them, the expression pathway is very important. Depending on the host cells and culture conditions, the types of HCPs vary greatly, ranging from hundreds to thousands. Many host cells such as E. coli, mammalian cells, NSO, SP2/0 and the human embryonic kidney cell line HEK293 have been used for biopharmaceutical production. During mammalian cell culture, recombinant proteins are often secreted from cells into cell culture fluid (CCF), which contains HCPs. In addition, due to the death of some cells, soluble intracellular proteins are released into CCF, and some artificial operations (such as centrifugation, filtration, etc.) can also cause cell lysis. Therefore, harvested CCF usually contains secreted HCPs and intracellular HCPs. When this protein mixture is incubated in a fermenter, other changes in HCPs occur due to enzymatic activity (such as proteases or sialidases).
The main factors affecting HCPs are shown in the table below:
Production ProcessInfluencing Factors of HCPsUpstream ProcessesAmino Acid Sequence of Drug Protein Host Cell Culture Process(Media Composition,Feeding Method, Temperature) Cell Viability at Harvest Time Of Culture Cells Amplification ProcessDownstream ProcessesCell Stability/Shear Sensitivity Purification Process Conditional Changes During Analysis
HCPs analysis provides information about the composition of substances entering the downstream process and the removal rate of HCPs at each purification step. In some cases, HCPs can even be combined with or co-purified with certain protein drugs. Process characterization and validation studies are needed to illustrate which process steps can remove HCPs and also to demonstrate the stability of these steps in removing HCPs. Therefore, detection of HCPs is an important part of purification process development and helps ensure production consistency. Finally, stable and highly sensitive detection methods are needed to detect HCPs of drug proteins.
Taking the CHO expression system as an example to introduce the analysis method of HCPs:
Quality Control Content and Requirements
Currently, there is no unified international standard for cell limits for HCPs, and biopharmaceutical companies use risk control to control the cell volume of HCPs. After the production and purification of any genetically engineered drug, trace amounts of HCPs are usually found in the final drug protein. The US FDA stipulates that when using a highly sensitive method to detect HCPs in pharmaceuticals, the content should be lower than the relative value of the lower detection limit of 100ppm (100ng·mg-1 total protein), which is usually considered an important reference point for process development. HCPs levels should be monitored in: 1) preclinical batches used for toxicological evaluation; 2) all batches during clinical development; and 3) process validation samples during final production.
Research Methods
During process development and production, appropriate methods must be selected for the detection of impurities such as HCPs, and their quantitative methods have always received attention. Currently, qualitative or semi-quantitative methods may be sufficient for process sample and batch testing. Typically, methods used for HCPs analysis include immunoassay methods (such as Western Blot and ELISA) or other methods (such as electrophoresis and mass spectrometry), and multiple techniques can be studied in parallel or in combination. In addition, new detection methods have emerged but are not yet widely used due to their immaturity.
ELISA Method
Among methods for HCPs analysis, anti-HCPs-ELISA is considered the gold standard. This method (1-100ppm) is suitable for product development and process control. However, unlike conventional ELISA, the target of anti-HCPs ELISA is not single, and the total HCPs “antigen” is a complex protein group. Therefore, when producing HCPs antibodies/standard reagents, it is necessary to ensure: 1) a specific production cell line and production process; 2) its protein concentration must be accurately quantified. The general method for preparing HCPs antibodies is to use host cells containing empty expression vectors to prepare antigen-immunized animals, obtain antiserum, and isolate and purify polyclonal antibodies for ELISA detection. Since the immunogenicity of HCPs as antigens depends on factors such as the structure, properties, abundance, and relative molecular mass of the protein itself, there will be different detection results during the analysis process, which to a certain extent will lead to inaccurate quantitative results.
In addition, commercial kits cannot cover all process-specific HCPs and cannot identify changes in HCPs caused by process changes, etc. If other binding and detection antibodies are used, it is recommended to test the detection antibody coverage. HCPs coverage assessment helps evaluate the antibody’s ability to identify HCPs in the standard as well as those present in the manufacturing process and protein drug product. The design and validation of immunoassays for HCPs is a challenge due to: 1) the method has a narrow dynamic range (<100), long development cycle, high cost, and high risk of failure; 2) a wide variety of possible kinds of HCPs in genetically engineered drugs; 3 ) Generally, polyclonal antibody reagents are used for detection; 4) Different proteins have similar epitopes, leading to false positives; 5) Hook effect, high-abundance proteins lead to detection saturation; 6) The antigen composition of HCPs should be comprehensive enough to withstand changes in the normal production process of the product; 7) There is a lack of completely matching quantitative standards. Since the HCPs test is used to detect samples containing HCPs, any cross-reactivity between anti-HCPs antibodies and drug proteins will affect the test and lead to biased results. Therefore, contamination by HCPs antigens must be avoided. In the future, it can be expected that ELISA will remain the gold standard for detecting HCPs, but in order to make this detection method more accurate, it is crucial to select appropriate antibodies.
Gel Electrophoresis/Western-Blot Method
Gel electrophoresis is commonly used in biopharmaceutical development laboratories to perform semi-quantitative analysis of different proteins present in a sample. For HCPs analysis, one-dimensional SDS-PAGE gels do not have high resolution but are used in combination with Western-Blot. Two-dimensional electrophoresis (2-DE) is commonly used for upstream or downstream process development and characterization, with its enhanced ability to resolve different HCPs on a single gel. The principle of 2-DE is to separate based on isoelectric point (first dimension) first, and then separate based on size (second dimension). Spot analysis in gel does not require immunoblotting, avoids the problem of membrane transfer, and can achieve the separation of trace HCPs impurities and products. Provides approximate relative molecular mass and isoelectric point information of protein spots, but excess protein may obscure HCPs spots. Mass spectrometry is often used to further identify in-gel proteins. Often, gel electrophoresis is used as a complementary method for the detection of non-immunogenic HCPs.
Western-Blot is used for consistent screening of large numbers of samples and detection of unknown proteins that react with anti-HCPs antibodies. It is not only suitable for detecting HCPs, but also provides approximate information on the relative molecular weight of HCPs and can be used as part of a GMP control system. However, Western-Blot also has big problems: 1) It requires high-quality HCPs polyclonal antibodies; 2) A large amount of overloaded target proteins in the gel will cause non-specific staining of the bands, thereby masking the possible bands of HCPs; 3) SDS-induced protein denaturation may lead to the loss of conformational epitopes; 4) Western-Blot cannot accurately quantify HCPs, and the sensitivity of the experiment depends on the quality of the polyclonal antibody.
Proximity Ligation Analysis (PLA)
In the PLA experiment, oligonucleotide chains (i.e., PLA probes) are labeled on 2 antibodies targeting different epitopes. These probes are connected by ligase when they are close to each other, and then amplified by qPCR to quantify the target proteins (i.e. HCPs).
Biosensor Method
Researchers report the use of biosensors for the detection of typical impurities in biopharmaceutical production. Biosensors can measure target molecules online making them promising analytical tools in process analytical technology (PAT). However, unlike traditional immunoassays, biosensors require regeneration, so the use of weak-affinity antibodies is recommended, but at the expense of sensitivity.
Mass Spectrometry
In recent years, mass spectrometry (MS) has been increasingly used in the detection of HCPs to help identify possible risk factors and evaluate purification processes. Although ELISA is most commonly used to detect the total amount of HCPs, it cannot identify HCPs outside the detection range of the ELISA kit, and compared with traditional ELISA methods, the liquid chromatography mass spectrometry (LC-MS) method has a short development time, It can specifically confirm and quantify all HCPs, detect all impurity proteins in an unbiased manner, and has the advantages of high method dynamic range (up to 6 orders of magnitude) and fast method adjustment.




Comments