Denials are a persistent challenge in the world of medical billing. Healthcare providers frequently face claim rejections from insurance companies for various reasons—be it incorrect coding, missing documentation, or issues with patient eligibility. When these claims are denied, the clock starts ticking on how quickly the appeal process can begin to recover lost revenue. Fortunately, advancements in denial appeal management software have made it easier to handle denied claims, reduce administrative burdens, and ultimately enhance revenue recovery for healthcare organizations.
The Impact of Denial Claims on Healthcare Providers:
Claim denials are not just a minor inconvenience. They represent lost revenue and disrupt the entire billing cycle. According to industry reports, up to 10% of claims can be denied, and a significant portion of these claims never get appealed successfully. The reasons for denials vary, but each rejection means more work for healthcare providers who must track, manage, and correct mistakes.
Moreover, a manual approach to appeals can be inefficient and error-prone. Healthcare staff often have to juggle multiple systems and paperwork, increasing the chances of missed deadlines or incomplete information. Without a structured, streamlined system, denied claims can easily slip through the cracks, leading to prolonged delays in reimbursement.
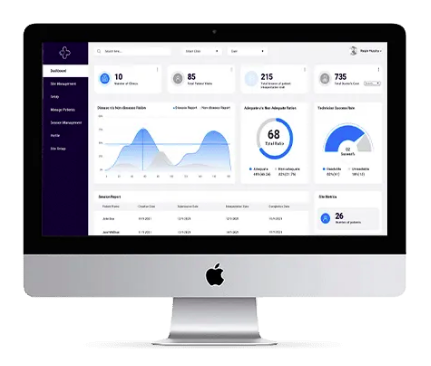
How Denial Management Software Works Denial appeal management software is a comprehensive solution that simplifies the process of identifying, managing, and appealing denied claims.
Key features of such software include:
- Real-Time Claim Tracking: This allows billing teams to track the status of denied claims in real time, providing a clear view of which claims are under appeal and which require further action. This transparency helps healthcare providers prioritize their efforts and resolve issues faster.
- Automated Appeal Generation: The software automates the creation of appeal documents, filling in necessary details, ensuring compliance with payer guidelines, and reducing the time spent on manual paperwork. This reduces administrative overhead and speeds up the appeals process.
- Root Cause Analysis: Advanced software includes analytics tools that help identify common causes of claim denials. Whether it's recurring issues with specific payers, coding errors, or authorization problems, these insights can guide billing teams to address the root causes, thus preventing future denials.
- Customizable Workflows: Different types of denials require different responses. Denial management software can be customized to fit the needs of each healthcare organization, providing tailored workflows that ensure each denial is handled according to its specific requirements.
Key Benefits for Healthcare Providers:
The advantages of using denial appeal management software are numerous:
- Faster Revenue Recovery: With automated appeals, real-time tracking, and streamlined workflows, providers can appeal claims more efficiently and recover lost revenue quicker.
- Reduced Denial Rates: By identifying trends in denied claims and improving the accuracy of billing and coding, healthcare providers can reduce the number of denials they receive.
- Improved Operational Efficiency: Automating repetitive tasks reduces the time and effort spent on manual processes, allowing staff to focus on more strategic tasks and patient care.
- Enhanced Financial Health: With fewer claims left unresolved and more timely appeals, practices can see a direct improvement in their cash flow and overall financial performance.
Conclusion:
Managing denied claims is a complex and time-sensitive task that requires precision, speed, and accuracy. Denial appeal management software offers healthcare providers a robust solution for tackling this issue, helping them streamline workflows, automate repetitive tasks, and ultimately reduce revenue loss. By incorporating advanced denial management tools into their billing processes, healthcare organizations can not only recover more lost revenue but also improve operational efficiency, reduce denial rates, and ensure smoother cash flow. In a competitive healthcare landscape, investing in such technology is a critical step toward maintaining financial sustainability and operational excellence.





Comments