Gabapentin 300 mg is a widely prescribed medication known for its effectiveness in managing various medical conditions, particularly those related to nerve pain and seizures. Understanding how gabapentin is supplied, including its dosage forms and strengths, is crucial for patients, caregivers, and healthcare providers to ensure its safe and effective use. This comprehensive guide delves into the details of gabapentin's active ingredient, available dosages, administration forms, and essential considerations for its use.
Introduction to Gabapentin
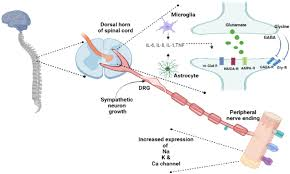
Gabapentin 800 mg, marketed under various brand names, such as Neurontin, is an anticonvulsant and neuropathic pain agent. Initially developed to treat epilepsy, its usage has expanded to address neuropathic pain, restless legs syndrome (RLS), and other off-label conditions. Its mechanism of action involves modulating the activity of neurotransmitters in the brain, thereby reducing the transmission of pain signals and stabilizing electrical activity in the nervous system.
Understanding the different ways gabapentin is supplied, including its milligram (mg) dosages and available formulations, is essential for optimizing therapeutic outcomes and minimizing potential risks.
Active Ingredient: Gabapentin
Gabapentin's chemical structure is similar to that of the neurotransmitter gamma-aminobutyric acid (GABA), although it does not directly interact with GABA receptors. Instead, gabapentin binds to the alpha-2-delta subunit of voltage-gated calcium channels in the central nervous system, which leads to decreased excitatory neurotransmitter release.
Key Properties:
- Chemical Name: 1-(aminomethyl)cyclohexaneacetic acid
- Molecular Formula: C₉H₁₇NO₂
- Mechanism of Action: Modulation of calcium channels, reducing excitatory neurotransmission.
Gabapentin is available only by prescription, emphasizing the importance of medical supervision during its use.
Dosage Forms of Gabapentin
Gabapentin is available in various dosage forms, each designed to accommodate different patient needs, preferences, and medical conditions. The primary forms include capsules, tablets, oral solutions, and extended-release tablets.
3.1. Capsules
Gabapentin capsules are one of the most common forms prescribed. They are available in several strengths, allowing for flexible dosing tailored to individual patient requirements.
- Sizes: Typically available in 100 mg, 300 mg, and 400 mg capsules.
- Advantages: Easy to swallow, pre-measured doses ensure accurate administration.
- Considerations: Capsules should be taken whole unless otherwise directed by a healthcare provider.
3.2. Tablets
Gabapentin tablets provide another option for oral administration, particularly suitable for patients who prefer not to use capsules.
- Sizes: Commonly available in 600 mg, 800 mg, and 1600 mg tablets.
- Advantages: Higher strength allows for fewer tablets per dose, which can enhance compliance.
- Considerations: Tablets should not be crushed or chewed unless specified, as this can alter the drug's release properties.
3.3. Oral Solution
The oral solution form of gabapentin is ideal for patients who have difficulty swallowing pills or require precise dosing adjustments.
- Concentrations: Typically available in 100 mg/mL and 200 mg/mL formulations.
- Advantages: Flexible dosing, easy administration for pediatric or geriatric patients.
- Considerations: Requires careful measurement using a proper dosing device to ensure accuracy.
3.4. Extended-Release Tablets
Extended-release (ER) gabapentin is designed to release the active ingredient slowly over time, allowing for once-daily dosing in some cases.
- Sizes: Commonly available in 600 mg and 900 mg extended-release tablets.
- Advantages: Reduced dosing frequency can improve adherence and smoother plasma concentration levels.
- Considerations: Should not be split, crushed, or chewed, as this can disrupt the extended-release mechanism.
Available Strengths
Gabapentin is supplied in a range of strengths to accommodate different therapeutic needs and patient profiles. The choice of strength depends on factors such as the condition being treated, patient age, kidney function, and response to therapy.
Capsules:
- 100 mg
- 300 mg
- 400 mg
Tablets:
- 600 mg
- 800 mg
- 1600 mg
Oral Solution:
- 100 mg/mL
- 200 mg/mL
Extended-Release Tablets:
- 600 mg
- 900 mg
Healthcare providers typically start patients on a lower dose, gradually increasing it to minimize side effects and assess tolerance.
How Gabapentin is Prescribed
Prescribing gabapentin involves a careful assessment of the patient's medical history, current condition, and potential for drug interactions. The dosing regimen is individualized, often starting with a low dose that is incrementally increased.
5.1. Starting Dosage
For adults with neuropathic pain or seizures, the initial dose is usually:
- Neuropathic Pain: 300 mg on Day 1, 300 mg twice daily on Day 2, and 300 mg three times daily on Day 3.
- Seizures: 300 mg on Day 1, 300 mg three times daily on Day 2, and 300 mg three to four times daily on Day 3.
5.2. Titration
After the initial days, the dose is typically increased based on patient response and tolerance. Titration aims to find the lowest effective dose that manages symptoms without causing significant side effects.
- Neuropathic Pain: The dose may be increased by 300 mg per day every few days.
- Seizures: Doses can be increased up to 1800 mg per day or more, divided into multiple doses.
5.3. Maintenance Dosage
Once the optimal dose is identified, it is maintained consistently to ensure ongoing symptom control.
- Neuropathic Pain: Common maintenance doses range from 900 mg to 3600 mg per day.
- Seizures: Maintenance doses often range from 1800 mg to 3600 mg per day, divided into three or four doses.
Adjustments may be necessary for patients with renal impairment, as gabapentin is primarily excreted unchanged by the kidneys.
Administration Guidelines
Proper administration of gabapentin is essential to maximize its therapeutic benefits and minimize adverse effects.
6.1. Timing
Gabapentin can be taken with or without food. However, taking it with food may help reduce gastrointestinal side effects such as nausea.
6.2. With or Without Food
- With Food: May enhance absorption and reduce stomach upset.
- Without Food: Absorption may be faster, which can be beneficial for some conditions.
6.3. Missed Doses
If a dose is missed, it should be taken as soon as possible. However, if it is close to the time for the next dose, skip the missed dose to avoid doubling up. Consistent dose schedules help maintain steady drug levels in the bloodstream.
Storage and Handling
Proper storage ensures the medication remains effective and safe for use.
- Temperature: Store at room temperature, away from excessive heat and moisture.
- Environment: Keep in a dry place, away from direct sunlight.
- Safety: Store gabapentin out of reach of children and pets to prevent accidental ingestion.
- Disposal: Unused or expired gabapentin should be disposed of according to local regulations, often through take-back programs or specific disposal instructions provided by pharmacists.
Potential Side Effects and Precautions
Like all medications, gabapentin can cause side effects, some of which may be serious. Understanding these potential adverse effects and taking necessary precautions is vital for safe usage.
Common Side Effects:
- Dizziness
- Drowsiness
- Fatigue
- Ataxia (loss of coordination)
- Peripheral edema (swelling of extremities)
- Nausea and vomiting
Serious Side Effects:
- Mood changes (e.g., depression, anxiety)
- Suicidal thoughts or behavior
- Severe allergic reactions (e.g., rash, itching, swelling, difficulty breathing)
- Respiratory depression, especially when combined with other CNS depressants
Precautions:
- Medical History: Inform your healthcare provider of any history of kidney disease, respiratory issues, or substance abuse.
- Pregnancy and Breastfeeding: Gabapentin should be used during pregnancy only if clearly needed, and caution is advised when breastfeeding.
- Operating Machinery: Due to its sedative effects, gabapentin may impair the ability to perform tasks that require alertness, such as driving.
Interactions with Other Medications
Gabapentin can interact with other medications, potentially altering its effectiveness or increasing the risk of adverse effects. It's essential to inform healthcare providers of all medications and supplements being taken.
Notable Interactions:
- CNS Depressants: Combining gabapentin with alcohol, benzodiazepines, opioids, or other sedatives can enhance drowsiness and respiratory depression.
- Antacids: Certain antacids containing aluminum or magnesium can reduce gabapentin absorption if taken simultaneously. It's advisable to space their administration by at least two hours.
- Morphine: Morphine can increase gabapentin absorption, potentially leading to higher plasma concentrations.
- Other Antiepileptic Drugs: Combining gabapentin with other anticonvulsants may require dosage adjustments and careful monitoring.
Mechanism of Interactions:
- Pharmacodynamic Interactions: Additive effects on the central nervous system can lead to enhanced sedation and respiratory depression.
- Pharmacokinetic Interactions: Changes in drug absorption or metabolism can affect gabapentin levels in the body.
Special Considerations
Certain populations require special attention when prescribing gabapentin to ensure safety and efficacy.
10.1. Pregnancy and Breastfeeding
- Pregnancy: Gabapentin is classified as a Category C drug by the FDA, indicating that risk to the fetus cannot be ruled out. It should be used during pregnancy only if the potential benefits justify the potential risks.
- Breastfeeding: Gabapentin is excreted in breast milk. Nursing mothers should consult their healthcare provider before using gabapentin.
10.2. Elderly Patients
- Increased Sensitivity: Older adults may be more sensitive to gabapentin's effects, such as dizziness and drowsiness, increasing the risk of falls.
- Dose Adjustments: Lower initial doses and gradual titration are recommended to minimize adverse effects.
- Renal Function: Age-related decline in kidney function may necessitate dosage adjustments to prevent accumulation and toxicity.
10.3. Pediatric Use
Gabapentin is approved for use in children for specific indications, such as seizures and neuropathic pain. Dosages must be carefully calculated based on the child's weight and response to therapy.
10.4. Renal Impairment
Since gabapentin is primarily eliminated by the kidneys, patients with renal impairment may require lower doses to prevent accumulation and toxicity. Regular monitoring of kidney function is essential.
Conclusion
Gabapentin is a versatile medication with a range of applications, particularly in managing neuropathic pain and seizures. Understanding how it is supplied, including its various dosage forms and strengths, is crucial for optimizing treatment outcomes. Patients should adhere strictly to prescribed dosages, be aware of potential side effects, and communicate openly with their healthcare providers about any concerns or other medications they are taking. With proper use and medical supervision, gabapentin can be an effective component of a comprehensive treatment plan for various neurological conditions.




Comments