Uterine cancer most often develops in the cells that form the endometrium, or lining of the uterus, which is a hollow, pear-shaped organ where fetal development takes place in a woman’s pelvis. Sometimes, due to abnormal changes in the cellular structure of the endometrium, new cells form when the body doesn’t need them, and old or damaged cells don’t die when they should. The resulting accumulation of excess cells can form a malignant, or cancerous, tumor, which can be serious if not treated properly. Endometrial cancer cells can also break away and travel to other parts of the body.
Discover personalized care and advanced treatment options for endometrial cancer treatment in Jaipur at Dr. Chandrakanta’s Gynae-Oncology Center. Led by renowned Gynae Oncologist, Dr. Chandrakanta, our center offers comprehensive and compassionate care tailored to each patient’s unique needs. With a focus on the latest advancements in gynecologic oncology, we strive to empower women through every step of their treatment journey. Trust in our expertise and dedication to guide you towards the best possible outcome.
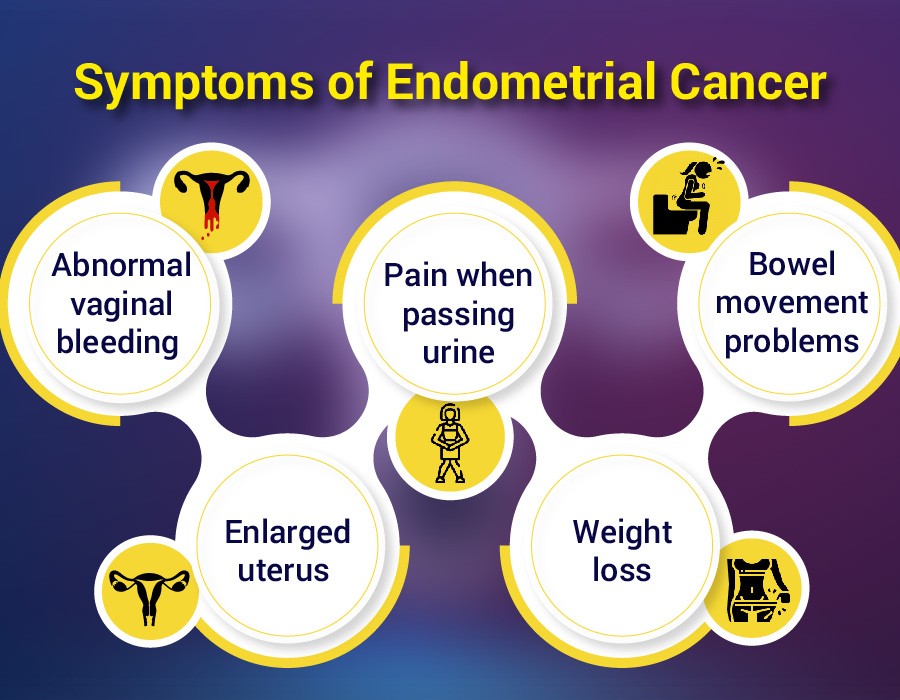
Signs and symptoms of uterine cancer
The most common sign of uterine cancer is abnormal vaginal bleeding — that is, bleeding that occurs between menstrual cycles or after menopause for older women. If you’re experiencing this type of bleeding, it’s important to speak with your gynecologist or physician right away to get to the bottom of this abnormality. Other symptoms of uterine cancer include irregular vaginal discharge, pain while urinating, unexplained weight loss, pelvic discomfort and anemia.
Risk factors of uterine cancer

While the exact cause of uterine cancer has yet to be discovered, researchers have identified several risk factors that increase a woman’s chance of being diagnosed with this condition. They include:
Being overweight or obese
Being older than 50
Having trouble getting pregnant
Having fewer than five periods a year before going through menopause
Taking estrogen-only hormone replacement therapy after menopause
Having excess estrogen exposure due to early-onset menstruation, never giving birth and/or late-onset menopause
Taking tamoxifen, a hormonal therapy used to treat or reduce the risk of breast cancer
Having a first-degree relative (mother, sister or daughter) with endometrial cancer
How uterine cancer is diagnosed
Uterine cancer is not typically detected through a routine Pap smear, as it develops in a woman’s uterus. (Pap smears generally only detect cervical cancers.) That’s why it’s important to talk to your physician if you’re experiencing abnormal vaginal symptoms, so that he or she can conduct additional testing of your endometrial tissue. Some of the different ways to test for uterine cancer include:
Endometrial biopsy — A small amount of endometrial tissue is removed using a thin, flexible tube that is inserted through the cervix and into the uterus.
Dilation and curettage — The uterus is dilated and a small, spoon-shaped instrument is inserted into the uterus to remove tissue.
Hysteroscopy — The uterus is filled with saline solution and a tiny telescope is inserted through the cervix so that a physician can closely look at the uterus and gather samples.
Stages of uterine cancer
Staging describes the extent to which the cancer has spread in the body and helps oncologists determine the optimal treatment plan for their patients. Uterine cancer has five stages, which include:
Stage 0 — Pre-invasive cancer cells are found on the surface of uterine cells but have not spread.
Stage 1 — Cancer is limited to the uterus.
Stage 2 — Cancer has spread to the cervix.
Stage 3 — Cancer has spread beyond the uterus to various structures of the pelvic region, most likely the ovaries, fallopian tubes, vagina or nearby lymph nodes.
Stage 4 — Cancer has spread to the bladder and/or rectum or to distant lymph nodes or organs.
Treating uterine cancer
Uterine cancer is most commonly treated with surgery followed by chemotherapy, radiation therapy and/or hormone therapy. These additional cancer therapies are completed even if the surgeon was able to remove the entire tumor to help ensure that any residual cancer cells are destroyed. Surgical options typically include:
Hysterectomy, which removes the uterus and cervix
Bilateral salpingo-oophorectomy, which removes the ovaries and fallopian tubes
Radical hysterectomy, which removes the uterus and cervix as well as part of the vagina and, possibly, the ovaries, fallopian tubes and nearby lymph nodes
Pelvic exenteration, which removes the uterus, cervix, vagina, ovaries, bladder, rectum and surrounding lymph nodes




Comments