Determining if a patient is a suitable candidate for penile surgery involves a comprehensive assessment by a penile surgeon, often a urologist specializing in genital reconstruction or sexual medicine.
The decision is based on several factors to ensure the procedure is safe and likely to achieve the desired outcomes for the patient.
1. Medical History Review: The first step for a penile surgeon is to review the patient’s medical history. This includes details about any existing medical conditions such as diabetes, hypertension, or cardiovascular disease, which may affect surgical outcomes or increase the risk of complications. Past surgeries and medications are also important considerations.
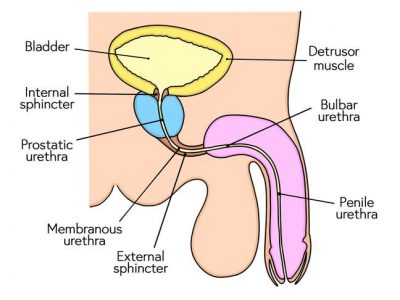
2. Physical Examination: A thorough physical examination of the genital area is conducted to assess the anatomy of the penis, scrotum, and surrounding tissues. This helps the surgeon evaluate the current state of the penis, including any deformities, scars, or conditions that may require correction or enhancement through surgery.
3. Diagnostic Tests: Depending on the specific reason for surgery, diagnostic tests such as blood tests, imaging studies (like ultrasound or MRI), or specialized penile function tests (such as Doppler ultrasound for erectile dysfunction) may be ordered. These tests provide objective data on penile function, blood flow, and anatomical structure, aiding in surgical planning.
4. Psychological Assessment: For procedures related to sexual function or aesthetics, a psychological assessment may be recommended. This helps ensure that the patient has realistic expectations about the outcomes of surgery and is mentally prepared for the procedure and potential changes in body image or sexual function.
5. Patient Goals and Expectations: Understanding the patient’s motivations for seeking penile surgery is crucial. Whether the goal is functional improvement (e.g., correction of Peyronie’s disease or erectile dysfunction) or cosmetic enhancement (e.g., penile lengthening or girth enhancement), the surgeon discusses expected outcomes, risks, and limitations of the procedure.
Patient consent is based on a clear understanding of what can be achieved through surgery.
6. Overall Health and Lifestyle Factors: The patient’s overall health and lifestyle habits, such as smoking, alcohol consumption, and physical activity levels, are assessed. Lifestyle factors can impact healing after surgery and may need to be addressed or modified preoperatively to optimize surgical outcomes and minimize risks.
7. Risks and Benefits Discussion: The penile surgeon discusses potential risks associated with the specific surgical procedure, such as infection, bleeding, scarring, and changes in sensation or function. They also outline the anticipated benefits and any alternatives to surgery, ensuring the patient can make an informed decision about proceeding with the procedure.
8. Follow-up Care and Long-Term Management: Before surgery, the surgeon outlines the postoperative care plan, including recovery expectations, follow-up appointments, and any necessary lifestyle adjustments. Long-term management may involve ongoing monitoring and potential adjustments to optimize outcomes.
In conclusion, determining candidacy for penile surgery involves a thorough assessment of medical history, physical examination, diagnostic tests, psychological evaluation, and discussions about patient goals and expectations. Collaboration between the patient and penile surgeon is essential to ensure that the chosen procedure is appropriate, safe, and likely to achieve satisfactory outcomes.




Comments