Introduction:
Gynaecological surgeries encompass a broad spectrum of procedures aimed at addressing various conditions affecting the female reproductive system. These surgeries are often necessary to alleviate symptoms, treat diseases, and improve overall health and quality of life. Understanding the causes behind these surgeries is crucial for women’s health awareness and informed decision-making. In this blog post, we delve into the common causes of gynaecological surgeries, the procedures involved, and what to expect during the recovery process.
Causes of Gynaecological Surgeries:
1. Fibroids : Uterine fibroids are noncancerous growths that can cause heavy menstrual bleeding, pelvic pain, and pressure symptoms. When fibroids become symptomatic and conservative treatments fail, surgical intervention such as myomectomy (removal of fibroids) or hysterectomy (removal of the uterus) may be necessary.
2. Endometriosis : Endometriosis is a condition where tissue similar to the lining of the uterus grows outside the uterus, leading to pelvic pain, painful periods, and infertility. Surgical options for endometriosis include laparoscopic excision of endometrial implants or laparoscopic hysterectomy in severe cases.
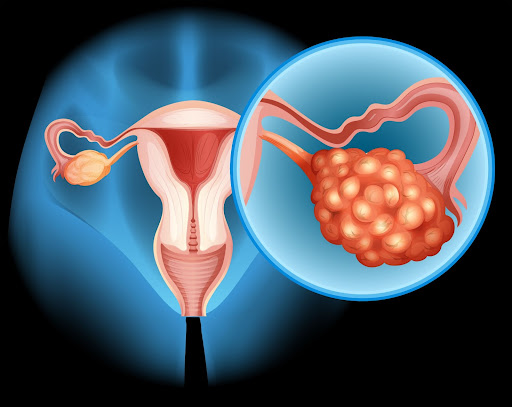
3. Ovarian Cysts : Ovarian cysts are fluid-filled sacs that develop on the ovaries. While many cysts resolve on their own, larger or persistent cysts may require surgical removal, especially if they are causing pain, bleeding, or torsion (twisting) of the ovary.
4. Pelvic Organ Prolapse : Pelvic organ prolapse occurs when the pelvic organs (such as the bladder, uterus, or rectum) descend into the vaginal canal due to weakened pelvic floor muscles. Surgical repair, known as pelvic organ prolapse surgery, aims to restore the normal position and function of the affected organs.
5. Pelvic Inflammatory Disease (PID): PID is an infection of the female reproductive organs, often caused by sexually transmitted bacteria. In severe cases where antibiotics are ineffective or if abscesses develop, surgery may be required to drain the abscesses and remove damaged tissue.
6. Cervical or Uterine Cancer: Surgical treatment for cervical or uterine cancer may involve removal of the cervix (trachelectomy), uterus (hysterectomy), and surrounding tissues. In some cases, lymph nodes in the pelvis may also be removed to assess the extent of cancer spread.
1. Laparoscopy: Laparoscopic surgery, also known as minimally invasive surgery, involves making small incisions in the abdomen through which a laparoscope (thin, flexible tube with a camera) and surgical instruments are inserted. This technique allows for shorter recovery times, less scarring, and reduced postoperative pain compared to traditional open surgery.
2. Hysteroscopy: Hysteroscopy involves the insertion of a hysteroscope (thin, lighted tube) through the vagina and cervix into the uterus to visualize and treat abnormalities such as fibroids, polyps, or adhesions. It can often be performed on an outpatient basis with minimal discomfort.
3. Robotic Surgery: Robotic-assisted surgery utilizes advanced robotic technology to enhance the precision and dexterity of surgical instruments. Surgeons control robotic arms from a console, allowing for greater maneuverability in tight spaces such as the pelvis.
4. Open Surgery: In cases where laparoscopic or robotic techniques are not feasible or appropriate, open surgery (laparotomy) may be performed, involving a larger abdominal incision. Open surgery is typically reserved for complex cases or when extensive tissue manipulation is required.
Recovery from Gynaecological Surgeries:
The recovery process following gynaecological surgery varies depending on the type and complexity of the procedure performed. However, there are some general guidelines that apply to many patients:
- Pain Management: Pain medication prescribed by your surgeon will help alleviate discomfort during the initial recovery period. Over-the-counter pain relievers may also be recommended.
- Rest and Activity: It’s essential to balance rest with light activity to promote healing and prevent complications such as blood clots. Your surgeon will provide guidance on when it’s safe to resume daily activities and return to work.
- Follow-up Care: Attend all scheduled follow-up appointments with your healthcare provider to monitor your progress, address any concerns, and ensure proper healing.
- Diet and Nutrition: Eat a well-balanced diet rich in nutrients to support recovery and promote tissue healing. Stay hydrated and avoid heavy or greasy foods that may cause digestive discomfort.
- Incision Care: Keep surgical incisions clean and dry to prevent infection. Follow your surgeon’s instructions regarding wound care, including showering and dressing changes.
- Physical Therapy: Depending on the type of surgery performed, your surgeon may recommend pelvic floor exercises or physical therapy to improve strength, flexibility, and bladder control.
Gynaecological surgeries play a vital role in managing various reproductive health conditions, offering relief from symptoms and improving overall well-being. By understanding the causes of these surgeries, the procedures involved, and what to expect during recovery, women can make informed decisions about their healthcare and take an active role in their recovery journey. Always consult with a qualified healthcare provider to discuss treatment options and develop a personalized care plan tailored to your individual needs.




Comments